Podiatry Network Solutions (PNS) has specific claim submission guidelines which requires 3 character Network ID (Carrier Designation) code is submitted in box 11c for paper claims and Loop 2000B SBR03 in the electronic claims. Each of the health plans has an assigned code. Previously these codes were hard coded by the Payer ID and Insurance entry name in each of these programs.
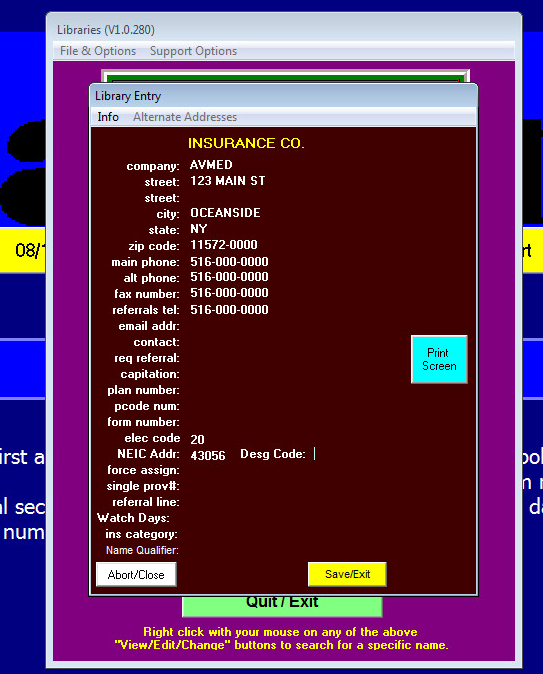
The insurance library (from the Libraries menu only) will now show the Desg Code when the assigned payer ID's for Podiatry Network Solutions are entered in the NEIC address of the insurance entry. (See the current table below). There is a validation when these payer ID's are added and you will be required to enter a valid designation code.
The Desg code will only be visible in from the Insurance Library. (not from the patient chart).
As of September 27, 2016 this is the current listing of Health Plans for PNS.
| Payer ID | Health Plan Name | Designation Code |
|---|---|---|
| 43056 | Health Options | PBC |
| 43056 | AvMed | PAV |
| 43056 | BCBS | PBC |
| 43056 | Magellan | PMA |
